How does your work support a better understanding of the treatment and/or prevention of diabetes?
Type 2 diabetes is by far the most common type of diabetes, and the cause is typically onset of metabolic disease due to obesity. We are interested in how increased adiposity (or fat mass in the body) leads to the disease of obesity, by asking how adipose stays healthy even as it expands versus becoming dysfunctional. Once adipose tissue is implicated, obesity causes numerous co-morbidities affecting nearly every organ and tissue in the body – so it is an important point of intervention. We are particularly interested in the role that the nerves and vasculature play to support healthy functions of adipose tissue. For example, we were the first to demonstrate that obesity and aging lead to a loss of proper nerve supply in adipose tissue (what we call ‘adipose neuropathy’), a finding that has now been shown by other research groups as well. Since we know from experimental models that loss of adipose nerves negatively impacts tissue and whole-body metabolic functions, we want to learn more about the physiology and pathophysiology of this adipose nerve supply, which provides important bi-directional neural communication with the brain. This is also important because peripheral neuropathy can be caused by obesity and diabetes, and impacts numerous tissues and organs that lose nerve supply, which we now know also includes adipose. Diabetes is the #1 cause of neuropathy overall, and has limited diagnostic and treatment options.
What innovative methodology are you using in your research?
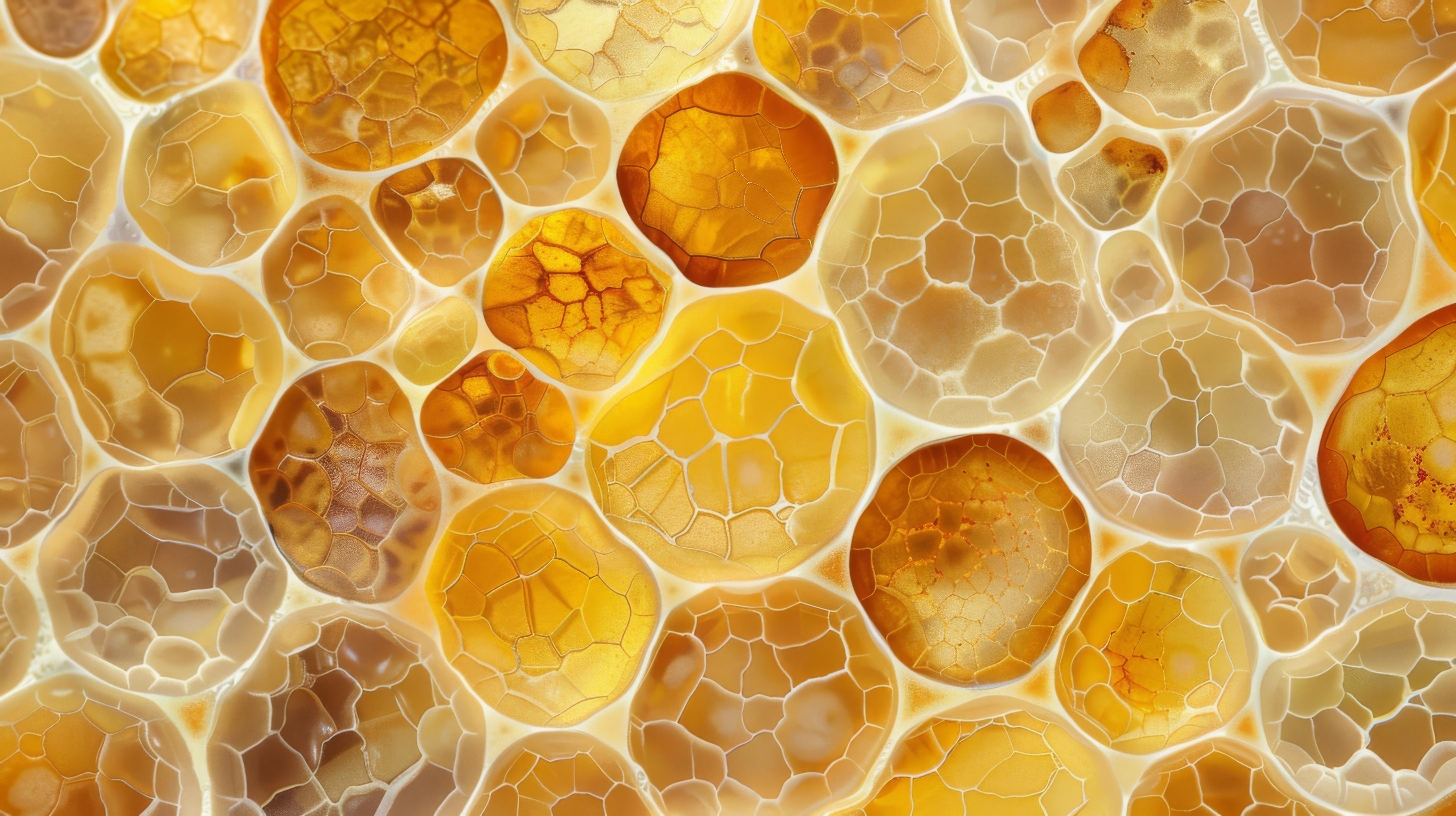
One thing we do is advanced microscopy imaging of the nerves in adipose, a method that led a member of my lab to discover the first-identified nerve terminal structure in adipose, which we call the ‘neuro-adipose nexus’ or NAN. NANs look like a web of nerve endings wrapping around a single adipocyte. We now know these NANs are sensory structures, ‘nociceptors’ actually, a sensory nerve subtype that responds to noxious stimuli such as inflammation. We are now using viral vectors, transgenic mouse lines, and molecular neuroscience techniques in combination to unravel how nerves in adipose stay healthy, and how they function or become dysfunctional. This includes investigating the sensory nerves in the tissue, which are poorly understood, and which we recently found can respond to local lipids and are the first to die with diet-induced adipose neuropathy.
What are the challenges related to this type of research?
These types of experiments are time-consuming, expensive, and require specially trained personnel who utilize highly-optimized and validated protocols. But we think this level of complexity and rigor is key to making pivotal discoveries and improving our understanding of how the nervous system impacts metabolic health or disease. Right now we have a stellar team in my lab, comprised of laboratory staff, postdoctoral fellows, graduate students, and undergraduate students, and together we prioritize team science, collaboration, and creativity in our work. This approach helps us move forward, even in uncertain funding climates or when experiments take longer than anticipated due to technical challenges, because we are passionate about the science and our approach to the research questions.
What excites you most about this research?
I am a Neuroscientist by training, and previously worked in the hypothalamus (the brain’s energy balance control and command center), and in adipose tissues. When I started by own lab in 2013, I decided to merge these interests and expertise to investigate neural communication and coordination of adipose functions. This decision turned out to be an important one, and I remain very excited about our research focus. We still do work on the hypothalamus and adipose tissues, but our research now merges these different fields, and we are seeing fascinating connections among them. Overall, the peripheral nervous system (PNS) is under-studied, and diseases that impact the PNS, such as peripheral neuropathies (which impact more than 30 million Americans alone), need much more research attention. We are grateful every day to be able to work across these disciplines, and get more researchers excited about looking at the peripheral nerve implications of their work.
How important is interdisciplinary collaboration to your research, and what programs and centers at OSU have assisted you in finding collaborators outside of your field?
We were recruited to Ohio State in 2020, and being here for the past 4 years has had hugely positive impacts on our research program. We now do more in the innovation space, and have numerous provisional patents for various discoveries (treatments, devices and biomarkers). We also now have clinical collaborations with neurological surgeons, neurologists, and psychiatrists that help improve our work and allow us to realize the ‘translational potential’ of our findings. We have collaborations on campus across the DHLRI, FFH, NRI, CCC, BME, and more.
Who are your primary collaborators?
At Ohio State we work closely with Drs. Martha Belury, Andrea Tedeschi, Kymberly Gowdy, Kristin Stanford, John McGregor, Brian Dalm, Bogdan Beirowski, and more.
Any closing thoughts?
If anyone is interested in innovation research, or moving their research projects to products that can have intellectual property (IP) protection and then be licensed or commercialized, please keep your eye out for the Research Accelerator Program to Translate, Innovate and Commercialize (RAPTIC). I created this program with numerous partners while serving as Director of Women in Medicine and Science in COM. We are now working with groups across campus to expand RAPTIC to all health, medical and biomedical faculty in any college, starting in summer 2025.
Interested in this area of research? Dr. Kristy Townsend and her collaborators will be hosting two events through The Ohio State University College of Medicine, where related projects will be presented. See below for further information: